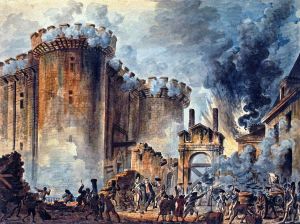
Fin de regime? Financial analysts are worried, après moi, le deluge… (Art courtesy fine folks at WikiMedia Commons.)
Good morning, ProviderNation. Political economy has long been known as “the dismal science.” But some things are true even if Lord Halifax says they are, and a great many of those who follow the economics of long term and post-acute care are asking themselves, “Where have all the good times gone?”
Despite a record fourth quarter for mergers or acquisitions, “it looks as if M&A fever may have broken,” the fine folks at Irving Levin Associates say, gloomily, in their latest report. “This could be the start of something small.”
We’ve covered some of the concerns about a demographic dip at length in this space. Another factor, though, is that old Washington bugbear (which we’ve also covered at length), regulatory certainty. It’s not so much the scale of changes that are happening—it’s the pace.
Regulatory Squeeze
“I didn’t think it could get worse, but it’s going to do,” says Irving Stackpole, a veteran analyst and my own, private Eeyore. “It’s going to get worse because of pressure by CMS to move from volume-based payments to value-based payments.”
It’s notorious, Stackpole and others say, that providers have built their businesses around a large Medicaid population, subsidized by a lower Medicare population with higher turnover. Now, though, the margins are being squeezed from both ends.
Just last month, a key congressional committee passed a bill that would reduce the amount states can collect in provider taxes. It could cost up to 20 states more than $8 billion in Medicaid revenue (because of the various perversities of the current system).
Meanwhile, regulators are speeding through their massive Rules of Participation rulemaking, and Congress is weighing even further value-based purchasing bill for Medicare. The Rules of Participation alone could cost care centers up to $75,000 apiece, advocates at the American Health Care Association say.
Well, now, say all the dismal scientists, that’s how the game works—some win and some lose. Except, for Stackpole and others, those who are bound to lose are those who don’t have much to begin with.
“The SNFs that are serving the most vulnerable populations, those SNFs are going to go bust,” Stackpole tells me. “We’re going to see even more closures, more beds come offline.”
Small/Independent Jeopardy
Stackpole is not on an island here, either. AHCA’s own James Michel, who it must be said is not easily ruffled, says he’s worried, too.
“We are particularly concerned about access in smaller and rural communities where there may only be one or a handful of facilities operating. CMS’ new payment models are rooted in risk-bearing models that make it very difficult, if not impossible, for smaller and independent facilities to participate successfully while keeping their autonomy,” Michel tells me in an email.
“While highly competitive markets can bear some degree of consolidation and constriction of the market, because the demand can be absorbed by the competition,” he adds, “smaller and rural markets with fewer providers certainly cannot. And even if they could, that isn’t necessarily a good thing. There is a growing area of research on the relationship between provider and payer consolidation, and increasing health care costs. In its attempt to constrain growing health care costs, CMS inadvertently may be promoting payment and delivery models that reward consolidation and force the closure of smaller facilities, thereby increasing overall costs and creating access problems for our most vulnerable populations.”
But don’t worry too much, because it can get worse, Michel adds.
‘Silver Tsunami’
“All of this is happening as we teeter on the edge of the ‘silver tsunami,’ where we are set to experience a rapid growth in the number of older Americans who will need long term care,” Michel says. “Are we shooting ourselves in the foot by adopting payment and delivery models that will result in a constriction of our long term care infrastructure at a time when we are going to most need it?”
The regulatory trends are frightening enough. But consider, again, the apparent cooldown in Wall Street’s ardour for seniors housing. What we’re all witnessing is money fleeing a sector from all sides. And that’s before we even consider the seismic shakeup we may be facing as younger adults wake up to their own history.
“If you have a 25-plus-percent under- or unemployment rate among millennials, redistribution will happen around invested capital. What would come out of the system is the capital invested in the insurance sector—a huge amount of the $2.7 trillion that’s spent goes into the pocket of some very well-heeled insurance companies—and that’s where the pushback comes from,” Stackpole says. “How could that surprise you?”
‘A Race To The Bottom’
All of this is completely predictable, but rather dismal, to contemplate, Stackpole says.
“Consolidation is the hallmark of a mature business life cycle,” he says. “And that’s where we are. You could not find a better example of a business cycle moving from its early maturing to its late decline than skilled nursing. You’ve got consolidation, you’ve got closure, you’ve got growing awareness in the market—these are all hallmarks of a profession in late decline.”
But the rubber, inevitably must meet the road.
“The people who really need that nursing center are the families of people who have neurological disorders, the families of people who have Alzheimer’s and dementia, and the people who really need a cardiac or a pulmonary rehab,” Stackpole says. “What they’re going to have to do now is drive 65, 70 miles. Does that matter? Maybe not to some guy at CMS in Baltimore, but to the rest of those people, it sure as hell does.”
So, if you happen to bump into Irving at some conference or other, make sure you buy him a drink or two. He could certainly use it.
“It’s a race to the bottom,” he says. “An absolute race to the bottom.”
Mad Props Dept.
On that cheery note, a couple/three bouquets to throw out.
First, to the fine folks at It’s Never 2 Late, who this week have entered their 2,000th care center.
Second, to the good people at Benchmark Senior Living, who’ve just been named the Boston area’s healthiest employer.
Finally, to Delaware’s own Susan M. Levy, MD, who has just been named president of AMDA—The Society for Post-Acute and Long-Term Care.
Bill Myers is Provider’s senior editor. Email him at wmyers@providermagazine.com. Follow him on Twitter, @ProviderMyers.













